Information for Parents & Carers
What is ‘CPIP’?
CPIP (Cerebral Palsy Integrated Pathway) is a follow-up programme for children with cerebral palsy or suspected cerebral palsy, allowing early detection of changes in muscles and joints with the option of earlier treatment for your child. This may help prevent problems developing in the future. At Chesterfield we also offer our CPIP assessments to any children whom present with similar conditions due to the assessment benefits.
What is Cerebral Palsy?
Cerebral Palsy (CP) is the term used for the physical disorder caused by brain injury or dysfunction occurring before the age of two. There are many different causes of cerebral palsy and the degree of functional impairment varies in each child from nearly normal function, to pronounced functional impairment.
Children with cerebral palsy often have increased tone (spasticity) in certain muscles while other muscles may be weakened. This can interfere with children’s ability to move and to learn to walk. Spasticity can also cause pain, and, over time, shortening of muscles and tendons. When joints do not move normally they become permanently stiff because the soft tissues tighten around them (known as a contracture).
In some children, the imbalance in the hip joint can lead to pulling of the head of the thigh bone out of its position in the hip joint leading to hip dislocation. Imbalance in the back, can lead to a curved spine or scoliosis. There are many different treatment methods to decrease spasticity and to prevent contractures and hip dislocation. These may include exercise or stretching and positioning programmes from your
physiotherapist, the use of splints during the day or at night or drug treatments to reduce the tightness in muscles. This does not describe all the treatments available. It is very important that the right treatments are available at an early stage to help prevent problems developing in order to achieve the best possible outcome.
What is the purpose of CPIP?
The purpose of CPIP is to ensure that children with risk of developing contractures or hip dislocation are detected early enabling timely intervention. The goal is that no child should be affected by severe contractures or hip dislocation and that every child should achieve the best function possible. Research has shown that x-rays of the hip taken at the right time can help us to spot this problem earlier – and take steps to reduce the chance of it getting worse.
The follow-up within CPIP involves the child’s physiotherapist who will make an assessment of the child’s muscle tone, joint motion, ability and function twice a year until the child is aged six. After that, an annual assessment is made until the child reaches adulthood. These assessments help the physiotherapist decide how often your child needs to be seen for treatment and what treatment options are best for
your child. Regular assessment and early treatment combine to improve outcomes.
X-rays
Children with CP should have an x-ray at 2 years of age. If your child is mildly affected you can expect one further x- ray aged 6 years. For those more severely affected there will be annual x-rays until age 8 years and then every other year. This is because there is a greater risk of dislocation in more severe cases. All children will be invited for a final x-ray at age 16.
How successful is CPIP?
Children treated under a similar programme in Sweden experienced significantly fewer hip dislocations. Significantly fewer children from this group developed contractures and scoliosis through participation in the programme. There was also a decrease in the number of major orthopaedic operations performed for hip dislocation and the cooperation between the different specialists involved in the care of children with cerebral palsy improved.
Participation
All the information from the CPIP assessments is stored in a secure NHS database. We can learn from experiences across Scotland to improve care in the future.
The child’s community paediatric team and doctor are able to get a CPIPS report, showing the child’s development over time and give warning signals showing when there is a need for intervention. This is fundamental in order to initiate the right treatment at the right time for each individual child.
Only anonymised information (that cannot be traced to you or your family) will be used in research. This means that a single child will never be identified when experiences from this follow-up programme are compiled into general reports. By carrying out research on the information available in the CPIPS database, we can improve our knowledge regarding changes over time in different types of cerebral palsy. The different treatments can be compared as to how they affect final outcome.
If you have any further questions regarding the information you have received please feel free to contact the Children’s Physiotherapy department
Hip surveillance are regular check-ups to monitor the position of a child’s hips. Sometimes a child’s hip can gradually move out of joint which can cause them problems. Hip surveillance aims to pick up on these problems early to allow appropriate management and better outcomes.
What hip problems are we looking for?
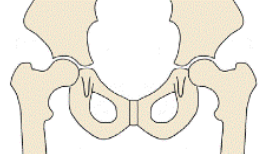
Typical hip: The hip is a ball and socket joint. The top of the thigh bone makes up the ball and part of the pelvis makes up the ‘socket’. In a healthy hip, the ball is completely covered by the socket.
Hip displacement: Hip displacement is when the ball gradually moves from under the socket. The more difficulty your child has with movement, particularly with standing and walking, the more at risk they of developing hip displacement. An X-ray is needed to see these changes.
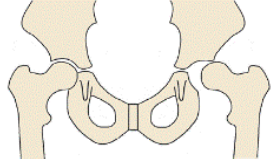
Hip dislocation:
Hip dislocation is when the ball has moved completely out from under the socket. With increasing hip displacement and dislocation, your child may have or develop: Pain decreased ability to move the hip, particularly taking their leg out to the side difficulty with personal care or toileting difficulty sitting or lying comfortably difficulty standing or walking pressure sores. Some children may have none of these signs or symptoms but still be experiencing changes to the position of their hips.
Who is hip surveillance important for?
Any child who is delayed in standing and walking can be at risk of developing hip problems. The more difficulty a child has with standing and walking, the greater the risk to their hips. Their hips can develop differently and will often have tight muscles making movements more difficult and encouraging them to rest in poor positions.
CPIP stands for the Cerebral Palsy Integrated Pathway. Children with Cerebral Palsy are at risk of developing hip problems. This is due to the impact their condition can have on their ability to stand and walk. The CPIP hip surveillance programme however is helpful for any child who has difficulty standing and walking regardless of their diagnosis.
If you are not sure if your child is at risk for hip displacement, please discuss with your child’s physiotherapist, or paediatrician.
What is involved in hip surveillance?
Hip surveillance includes assessments of your child’s hips by a physiotherapist and hip X-rays at scheduled times. Hip X-rays are taken to look at the position of the hip because hip displacement can happen without any signs or symptoms. Taking part in hip surveillance allows your child’s health care team to find hip displacement early and help your child before the hip becomes dislocated. The CPIP hip surveillance program for children is supported by an orthopaedic consultant, physiotherapist and sometimes their paediatrician at Sheffield Children’s Hospital who work together.